Dental caries
|
| |
| Destruction of a tooth by cervical decay from dental caries |
Dental caries, also known as tooth decay, is a disease where bacterial processes damage hard tooth structure (enamel, dentin and cementum). These tissues progressively break down, producing dental cavities (holes in the teeth). If left untreated, the disease can lead to pain, tooth loss, infection, and, in severe cases, death. Today, caries remains one of the most common diseases throughout the world.
The presentation of caries is highly variable, however the risk factors and stages of development are similar. Initially, it may appear as a small chalky area which may eventually develop into a large cavitation. Sometimes caries may be directly visible, however other methods of detection such as radiographs are used for less visible areas of teeth and to judge the extent of destruction.
Tooth decay is caused by specific types of acid-producing bacteria which cause damage in the presence of fermentable carbohydrates such as sucrose, fructose, and glucose. The mineral content of teeth is sensitive to increases in acidity from the production of lactic acid. Specifically, a tooth (which is primarily mineral in content) is in a constant state of back-and-forth demineralization and remineralization between the tooth and surrounding saliva. When the pH at the surface of the tooth drops below 5.5, demineralization proceeds faster than remineralization (i.e. there is a net loss of mineral structure on the tooth's surface). This results in the ensuing decay. Depending on the extent of tooth destruction, various treatments can be used to restore teeth to proper form, function, and aesthetics, but there is no known method to regenerate large amounts of tooth structure. Instead, dental health organizations advocate preventive and prophylactic measures, such as regular oral hygiene and dietary modifications, to avoid dental caries.
History

An image from 1300s (A.D.) England depicting a dentist extracting a tooth with forceps.
There is a long history of dental caries: over a million years ago, hominids such as Australopithecus suffered from cavities. The largest increases in the prevalence of caries have been associated with dietary changes. Archaeological evidence shows that tooth decay is an ancient disease dating far into prehistory. Skulls dating from a million years ago through the neolithic period show signs of caries, excepting those from the Paleolithic and Mesolithic ages. The increase of caries during the neolithic period may be attributed to the increase of plant foods containing carbohydrates. The beginning of rice cultivation in South Asia is also believed to have caused an increase in caries.
A Sumerian text from 5000 BC describes a "tooth worm" as the cause of caries. Evidence of this belief has also been found in India, Egypt, Japan, and China.
Unearthed ancient skulls show evidence of primitive dental work. In Pakistan, teeth dating from around 5500 BC to 7000 BC show nearly perfect holes from primitive dental drills. The Ebers Papyrus, an Egyptian text from 1550 BC, mentions diseases of teeth. During the Sargonid dynasty of Assyria during 668 to 626 BC, writings from the king's physician specify the need to extract a tooth due to spreading inflammation. In the Roman Empire, wider consumption of cooked foods led to a small increase in caries prevalence. The Greco-Roman civilization, in addition to the Egyptian, had treatments for pain resulting from caries.
The rate of caries remained low through the Bronze and Iron ages, but sharply increased during the Medieval period. Periodic increases in caries prevalence had been small in comparison to the 1000 AD increase, when sugar cane became more accessible to the Western world. Treatment consisted mainly of herbal remedies and charms, but sometimes also included bloodletting. The barber surgeons of the time provided services that included tooth extractions. Learning their training from apprenticeships, these health providers were quite successful in ending tooth pain and likely prevented systemic spread of infections in many cases. Among Roman Catholics, prayers to Saint Apollonia, the patroness of dentistry, were meant to heal pain derived from tooth infection.
There is also evidence of caries increase in North American Indians after contact with colonizing Europeans. Before colonization, North American Indians subsisted on hunter-gatherer diets, but afterwards there was a greater reliance on maize agriculture, which made these groups more susceptible to caries.
In the medieval Islamic world, Muslim physicians such as al-Gazzar and Avicenna (in The Canon of Medicine) provided the earliest known treatments for caries, though they also believed that it was caused by tooth worms as the ancients had. This was eventually proven false in 1200 by another Muslim dentist named Gaubari, who in his Book of the Elite concerning the unmasking of mysteries and tearing of veils, was the first to reject the idea of caries being caused by tooth worms, and he stated that tooth worms in fact do not even exist. The theory of the tooth worm was thus no longer accepted in the Islamic medical community from the 13th century onwards.
During the European Age of Enlightenment, the belief that a "tooth worm" caused caries was also no longer accepted in the European medical community. Pierre Fauchard, known as the father of modern dentistry, was one of the first to reject the idea that worms caused tooth decay and noted that sugar was detrimental to the teeth and gingiva. In 1850, another sharp increase in the prevalence of caries occurred and is believed to be a result of widespread diet changes. Prior to this time, cervical caries was the most frequent type of caries, but increased availability of sugar cane, refined flour, bread, and sweetened tea corresponded with a greater number of pit and fissure caries.
In the 1890s, W.D. Miller conducted a series of studies that led him to propose an explanation for dental caries that was influential for current theories. He found that bacteria inhabited the mouth and that they produced acids which dissolved tooth structures when in the presence of fermentable carbohydrates. This explanation is known as the chemoparasitic caries theory. Miller's contribution, along with the research on plaque by G.V. Black and J.L. Williams, served as the foundation for the current explanation of the etiology of caries. Several of the specific strains of bacteria were identified in 1921 by Fernando E. Rodriguez Vargas.
Epidemiology
Worldwide, most children and an estimated ninety percent of adults have experienced caries, with the disease most prevalent in Asian and Latin American countries and least prevalent in African countries. In the United States, dental caries is the most common chronic childhood disease, being at least five times more common than asthma. It is the primary pathological cause of tooth loss in children. Between 29% and 59% of adults over the age of fifty experience caries.
The number of cases has decreased in some developed countries, and this decline is usually attributed to increasingly better oral hygiene practices and preventive measures such as fluoride treatment. Nonetheless, countries that have experienced an overall decrease in cases of tooth decay continue to have a disparity in the distribution of the disease. Among children in the United States and Europe, twenty percent of the population endures sixty to eighty percent of cases of dental caries. A similarly skewed distribution of the disease is found throughout the world with some children having none or very few caries and others having a high number. Australia, Nepal, and Sweden have a low incidence of cases of dental caries among children, whereas cases are more numerous in Costa Rica and Slovakia.
The classic "DMF" (decay/missing/filled) index is one of the most common methods for assessing caries prevalence as well as dental treatment needs among populations. This index is based on in-field clinical examination of individuals by using a probe, mirror and cotton rolls. Because the DMF index is done without X-ray imaging, it underestimates real caries prevalence and treatment needs.
Classification
Caries can be classified by location, etiology, rate of progression, and affected hard tissues. These classification can be used to characterize a particular case of tooth decay in order to more accurately represent the condition to others and also indicate the severity of tooth destruction.
Location
Generally, there are two types of caries when separated by location: caries found on smooth surfaces and caries found in pits and fissures. The location, development, and progression of smooth-surface caries differ from those of pit and fissure caries. G.V. Black created a classification system that is widely used and based on the location of the caries on the tooth. The original classification distinguished caries into five groups, indicated by the word, "Class", and a Roman numeral. Pit and fissure caries is indicated as Class I; smooth surface caries is further divided into Class II, Class III, Class IV, and Class V. A Class VI was added onto Black's classification and also represents a smooth-surface carious lesion.

GV Black Classification of Restorations

The pits and fissures of teeth provide a location for caries formation.
Pit and fissure caries
Pits and fissures are anatomic landmarks on a tooth where the enamel folds inward. Fissures are formed during the development of grooves but the enamel in the area is not fully fused. As a result, a deep linear depression forms in the enamel's surface structure, which forms a location for dental caries to develop and flourish. Fissures are mostly located on the occlusal (chewing) surfaces of posterior teeth and palatal surfaces of maxillary anterior teeth. Pits are small, pinpoint depressions that are most commonly found at the ends or cross-sections of grooves. In particular, buccal pits are found on the facial surfaces of molars. For all types of pits and fissures, the deep infolding of enamel makes oral hygiene along these surfaces difficult, allowing dental caries to develop more commonly in these areas.
The occlusal surfaces of teeth represent 12.5% of all tooth surfaces but are the location of over 50% of all dental caries. Among children, pit and fissure caries represent 90% of all dental caries. Pit and fissure caries can sometimes be difficult to detect. As the decay progresses, caries in enamel nearest the surface of the tooth spreads gradually deeper. Once the caries reaches the dentin at the dentino-enamel junction, the decay quickly spreads laterally. Within the dentin, the decay follows a triangle pattern that points to the tooth's pulp. This pattern of decay is typically described as two triangles (one triangle in enamel, and another in dentin) with their bases conjoined to each other at the dentino-enamel junction (DEJ). This base-to-base pattern is typical of pit and fissure caries, unlike smooth-surface caries (where base and apex of the two triangles join).
Smooth-surface caries
There are three types of smooth-surface caries. Proximal caries, also called interproximal caries, form on the smooth surfaces between adjacent teeth. Root caries form on the root surfaces of teeth. The third type of smooth-surface caries occur on any other smooth tooth surface.

In this radiograph, the dark spots in the adjacent teeth show proximal caries.
Proximal caries are the most difficult type to detect. Frequently, this type of caries cannot be detected visually or manually with a dental explorer. Proximal caries form cervically (toward the roots of a tooth) just under the contact between two teeth. As a result, radiographs are needed for early discovery of proximal caries. Under Black's classification system, proximal caries on posterior teeth (premolars and molars) are designated as Class II caries. Proximal caries on anterior teeth (incisors and canines) are indicated as Class III if the incisal edge (chewing surface) is not included and Class IV if the incisal edge is included.
Root caries, which are sometimes described as a category of smooth-surfaces caries, are the third most common type of caries and usually occur when the root surfaces have been exposed due to gingival recession. When the gingiva is healthy, root caries is unlikely to develop because the root surfaces are not as accessible to bacterial plaque. The root surface is more vulnerable to the demineralization process than enamel because cementum begins to demineralize at 6.7 pH, which is higher than enamel's critical pH. Regardless, it is easier to arrest the progression of root caries than enamel caries because roots have a greater reuptake of fluoride than enamel. Root caries are most likely to be found on facial surfaces, then interproximal surfaces, then lingual surfaces. Mandibular molars are the most common location to find root caries, followed by mandibular premolars, maxillary anteriors, maxillary posteriors, and mandibular anteriors.
Lesions on other smooth surfaces of teeth are also possible. Since these occur in all smooth surface areas of enamel except for interproximal areas, these types of caries are easily detected and are associated with high levels of plaque and diets promoting caries formation. Under Black's classification system, caries near the gingiva on the facial or lingual surfaces is designated Class V. Class VI is reserved for caries confined to cusp tips on posterior teeth or incisal edges of anterior teeth.
Other general descriptions
Besides the two previously mentioned categories, carious lesions can be described further by their location on a particular surface of a tooth. Caries on a tooth's surface that are nearest the cheeks or lips are called "facial caries", and caries on surfaces facing the tongue are known as "lingual caries". Facial caries can be subdivided into buccal (when found on the surfaces of posterior teeth nearest the cheeks) and labial (when found on the surfaces of anterior teeth nearest the lips). Lingual caries can also be described as palatal when found on the lingual surfaces of maxillary teeth because they are located beside the hard palate.
Caries near a tooth's cervix—the location where the crown of a tooth and its roots meet—are referred to as cervical caries. Occlusal caries are found on the chewing surfaces of posterior teeth. Incisal caries are caries found on the chewing surfaces of anterior teeth. Caries can also be described as "mesial" or "distal." Mesial signifies a location on a tooth closer to the median line of the face, which is located on a vertical axis between the eyes, down the nose, and between the contact of the central incisors. Locations on a tooth further away from the median line are described as distal.
Etiology

Rampant caries as seen here may be due to methamphetamine use.
In some instances, caries are described in other ways that might indicate the cause. "Baby bottle caries", "early childhood caries", or "baby bottle tooth decay" is a pattern of decay found in young children with their deciduous (baby) teeth. The teeth most likely affected are the maxillary anterior teeth, but all teeth can be affected. The name for this type of caries comes from the fact that the decay usually is a result of allowing children to fall asleep with sweetened liquids in their bottles or feeding children sweetened liquids multiple times during the day. Another pattern of decay is "rampant caries", which signifies advanced or severe decay on multiple surfaces of many teeth. Rampant caries may be seen in individuals with xerostomia, poor oral hygiene, methamphetamine use (due to drug-induced dry mouth), and/or large sugar intake. If rampant caries is a result of previous radiation to the head and neck, it may be described as radiation-induced caries. Problems can also be caused by the self destruction of roots and whole tooth resorption when new teeth erupt or later from unknown causes.
Rate of progression
Temporal descriptions can be applied to caries to indicate the progression rate and previous history. "Acute" signifies a quickly developing condition, whereas "chronic" describes a condition which has taken an extended time to develop. Recurrent caries, also described as secondary, are caries that appears at a location with a previous history of caries. This is frequently found on the margins of fillings and other dental restorations. On the other hand, incipient caries describes decay at a location that has not experienced previous decay. Arrested caries describes a lesion on a tooth which was previously demineralized but was remineralized before causing a cavitation.
Affected hard tissue
Depending on which hard tissues are affected, it is possible to describe caries as involving enamel, dentin, or cementum. Early in its development, caries may affect only enamel. Once the extent of decay reaches the deeper layer of dentin, "dentinal caries" is used. Since cementum is the hard tissue that covers the roots of teeth, it is not often affected by decay unless the roots of teeth are exposed to the mouth. Although the term "cementum caries" may be used to describe the decay on roots of teeth, very rarely does caries affect the cementum alone. Roots have a very thin layer of cementum over a large layer of dentin, and thus most caries affecting cementum also affects dentin.
Signs and symptoms

Dental explorer used for caries diagnosis.
A person experiencing caries may not be aware of the disease. The earliest sign of a new carious lesion is the appearance of a chalky white spot on the surface of the tooth, indicating an area of demineralization of enamel. This is referred to as incipient decay. As the lesion continues to demineralize, it can turn brown but will eventually turn into a cavitation ("cavity"). Before the cavity forms, the process is reversible, but once a cavity forms, the lost tooth structure cannot be regenerated. A lesion which appears brown and shiny suggests dental caries was once present but the demineralization process has stopped, leaving a stain. A brown spot which is dull in appearance is probably a sign of active caries.
As the enamel and dentin are destroyed, the cavity becomes more noticeable. The affected areas of the tooth change color and become soft to the touch. Once the decay passes through enamel, the dentinal tubules, which have passages to the nerve of the tooth, become exposed and cause the tooth to hurt. The pain may worsen with exposure to heat, cold, or sweet foods and drinks. Dental caries can also cause bad breath and foul tastes. In highly progressed cases, infection can spread from the tooth to the surrounding soft tissues. Complications such as cavernous sinus thrombosis and Ludwig's angina can be life-threatening.
Diagnosis
Primary diagnosis involves inspection of all visible tooth surfaces using a good light source, dental mirror and explorer. Dental radiographs (X-rays) may show dental caries before it is otherwise visible, particularly caries between the teeth. Large dental caries are often apparent to the naked eye, but smaller lesions can be difficult to identify. Visual and tactile inspection along with radiographs are employed frequently among dentists, particularly to diagnose pit and fissure caries. Early, uncavitated caries is often diagnosed by blowing air across the suspect surface, which removes moisture and changes the optical properties of the unmineralized enamel. This produces a white 'halo' effect detectable to the naked eye. Fiberoptic transillumination, lasers and disclosing dyes have been recommended for use as an adjunct when diagnosing smaller carious lesions in pits and fissures of teeth.

(A) A small spot of decay visible on the surface of a tooth. (B) The radiograph reveals an extensive region of demineralization within the dentin (arrows). (C) A hole is discovered on the side of the tooth at the beginning of decay removal. (D) All decay removed.
Some dental researchers have cautioned against the use of dental explorers to find caries. In cases where a small area of tooth has begun demineralizing but has not yet cavitated, the pressure from the dental explorer could cause a cavity. Since the carious process is reversible before a cavity is present, it may be possible to arrest the caries with fluoride and remineralize the tooth surface. When a cavity is present, a restoration will be needed to replace the lost tooth structure.
At times, pit and fissure caries may be difficult to detect. Bacteria can penetrate the enamel to reach dentin, but then the outer surface may remineralize, especially if fluoride is present. These caries, sometimes referred to as "hidden caries", will still be visible on x-ray radiographs, but visual examination of the tooth would show the enamel intact or minimally perforated.
Causes
There are four main criteria required for caries formation: a tooth surface (enamel or dentin); caries-causing bacteria; fermentable carbohydrates (such as sucrose); and time. The caries process does not have an inevitable outcome, and different individuals will be susceptible to different degrees depending on the shape of their teeth, oral hygiene habits, and the buffering capacity of their saliva. Dental caries can occur on any surface of a tooth which is exposed to the oral cavity, but not the structures which are retained within the bone.
Teeth
There are certain diseases and disorders affecting teeth which may leave an individual at a greater risk for caries. Amelogenesis imperfecta, which occurs between 1 in 718 and 1 in 14,000 individuals, is a disease in which the enamel does not fully form or forms in insufficient amounts and can fall off a tooth. In both cases, teeth may be left more vulnerable to decay because the enamel is not able to protect the tooth.
In most people, disorders or diseases affecting teeth are not the primary cause of dental caries. Ninety-six percent of tooth enamel is composed of minerals. These minerals, especially hydroxyapatite, will become soluble when exposed to acidic environments. Enamel begins to demineralize at a pH of 5.5. Dentin and cementum are more susceptible to caries than enamel because they have lower mineral content. Thus, when root surfaces of teeth are exposed from gingival recession or periodontal disease, caries can develop more readily. Even in a healthy oral environment, however, the tooth is susceptible to dental caries.
The anatomy of teeth may affect the likelihood of caries formation. Where the deep grooves of teeth are more numerous and exaggerated, pit and fissure caries are more likely to develop. Also, caries are more likely to develop when food is trapped between teeth.
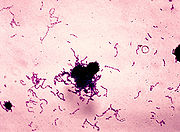
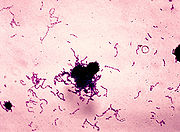
A gram stain image of Streptococcus mutans.
Bacteria
The mouth contains a wide variety of bacteria, but only a few specific species of bacteria are believed to cause dental caries: Streptococcus mutans and Lactobacilli among them. Lactobacillus acidophilus, Actinomyces viscosus, Nocardia spp., and Streptococcus mutans are most closely associated with caries, particularly root caries. Bacteria collect around the teeth and gums in a sticky, creamy-coloured mass called plaque, which serves as a biofilm. Some sites collect plaque more commonly than others. The grooves on the biting surfaces of molar and premolar teeth provide microscopic retention, as does the point of contact between teeth. Plaque may also collect along the gingiva. In addition, the edges of fillings or crowns can provide protection for bacteria, as can intraoral appliances such as orthodontic braces or removable partial dentures.
Fermentable carbohydrates
Bacteria in a person's mouth convert glucose, fructose, and most commonly sucrose (table sugar) into acids such as lactic acid through a glycolytic process called fermentation. If left in contact with the tooth, these acids may cause demineralization, which is the dissolution of its mineral content. The process is dynamic, however, as remineralization can also occur if the acid is neutralized by saliva or mouthwash. Fluoride toothpaste or dental varnish may aid remineralization. If demineralization continues over time, enough mineral content may be lost so that the soft organic material left behind disintegrates, forming a cavity or hole.
Time
The frequency of which teeth are exposed to cariogenic (acidic) environments affects the likelihood of caries development. After meals or snacks, the bacteria in the mouth metabolize sugar, resulting in an acidic by-product which decreases pH. As time progresses, the pH returns to normal due to the buffering capacity of saliva and the dissolved mineral content of tooth surfaces. During every exposure to the acidic environment, portions of the inorganic mineral content at the surface of teeth dissolves and can remain dissolved for 2 hours. Since teeth are vulnerable during these acidic periods, the development of dental caries relies heavily on the frequency of acid exposure. For example, when sugars are eaten continuously throughout the day, the tooth is more vulnerable to caries for a longer period of time, and caries are more likely to develop because the pH never returns to normal levels, thus the tooth surfaces cannot remineralize or regain lost mineral content.
The carious process can begin within days of a tooth erupting into the mouth if the diet is sufficiently rich in suitable carbohydrates. Evidence suggests that the introduction of fluoride treatments have slowed the process. Proximal caries take an average of four years to pass through enamel in permanent teeth. Because the cementum enveloping the root surface is not nearly as durable as the enamel encasing the crown, root caries tends to progress much more rapidly than decay on other surfaces. The progression and loss of mineralization on the root surface is 2.5 times faster than caries in enamel. In very severe cases where oral hygiene is very poor and where the diet is very rich in fermentable carbohydrates, caries may cause cavities within months of tooth eruption. This can occur, for example, when children continuously drink sugary drinks from baby bottles. On the other hand, it may take years before the process results in a cavity being formed.
Other risk factors
Reduced saliva is associated with increased caries since the buffering capability of saliva is not present to counterbalance the acidic environment created by certain foods. As a result, medical conditions that reduce the amount of saliva produced by salivary glands, particularly the submandibular gland and parotid gland, are likely to lead to widespread tooth decay. Examples include Sjögren's syndrome, diabetes mellitus, diabetes insipidus, and sarcoidosis. Medications, such as antihistamines and antidepressants, can also impair salivary flow. Moreover, sixty-three percent of the most commonly prescribed medications in the United States list dry mouth as a known side effect. Radiation therapy of the head and neck may also damage the cells in salivary glands, increasing the likelihood of caries formation.
The use of tobacco may also increase the risk for caries formation. Some brands of smokeless tobacco contain high sugar content, increasing susceptibility to caries. Tobacco use is a significant risk factor for periodontal disease, which can cause the gingiva to recede. As the gingiva loses attachment to the teeth, the root surface becomes more visible in the mouth. If this occurs, root caries is a concern since the cementum covering the roots of teeth is more easily demineralized by acids than enamel. Currently, there is not enough evidence to support a causal relationship between smoking and coronal caries, but evidence does suggest a relationship between smoking and root-surface caries.
Pathophysiology
The progression of pit and fissure caries resembles two triangles with their bases meeting along the junction of enamel and dentin.
Enamel
Enamel is a highly mineralized acellular tissue, and caries act upon it through a chemical process brought on by the acidic environment produced by bacteria. As the bacteria consume the sugar and use it for their own energy, they produce lactic acid. The effects of this process include the demineralization of crystals in the enamel, caused by acids, over time until the bacteria physically penetrate the dentin. Enamel rods, which are the basic unit of the enamel structure, run perpendicularly from the surface of the tooth to the dentin. Since demineralization of enamel by caries generally follows the direction of the enamel rods, the different triangular patterns between pit and fissure and smooth-surface caries develop in the enamel because the orientation of enamel rods are different in the two areas of the tooth .
As the enamel loses minerals , and dental caries progress, they develop several distinct zones, visible under a light microscope. From the deepest layer of the enamel to the enamel surface, the identified areas are the: translucent zone, dark zones, body of the lesion, and surface zone. The translucent zone is the first visible sign of caries and coincides with a 1-2% loss of minerals. A slight remineralization of enamel occurs in the dark zone, which serves as an example of how the development of dental caries is an active process with alternating changes. The area of greatest demineralization and destruction is in the body of the lesion itself. The surface zone remains relatively mineralized and is present until the loss of tooth structure results in a cavitation.
Dentin
Unlike enamel, the dentin reacts to the progression of dental caries. After tooth formation, the ameloblasts, which produce enamel, are destroyed once enamel formation is complete and thus cannot later regenerate enamel after its destruction. On the other hand, dentin is produced continuously throughout life by odontoblasts, which reside at the border between the pulp and dentin. Since odontoblasts are present, a stimulus, such as caries, can trigger a biologic response. These defense mechanisms include the formation of sclerotic and tertiary dentin.
In dentin from the deepest layer to the enamel, the distinct areas affected by caries are the translucent zone, the zone of bacterial penetration, and the zone of destruction. The translucent zone represents the advancing front of the carious process and is where the initial demineralization begins. The zones of bacterial penetration and destruction are the locations of invading bacteria and ultimately the decomposition of dentin.

The faster spread of caries through dentin creates this triangular appearance in smooth surface caries.
Sclerotic dentin
The structure of dentin is an arrangement of microscopic channels, called dentinal tubules, which radiate outward from the pulp chamber to the exterior cementum or enamel border. The diameter of the dentinal tubules is largest near the pulp (about 2.5 μm) and smallest (about 900 nm) at the junction of dentin and enamel. The carious process continues through the dentinal tubules, which are responsible for the triangular patterns resulting from the progression of caries deep into the tooth. The tubules also allow caries to progress faster.
In response, the fluid inside the tubules bring immunoglobulins from the immune system to fight the bacterial infection. At the same time, there is an increase of mineralization of the surrounding tubules. This results in a constriction of the tubules, which is an attempt to slow the bacterial progression. In addition, as the acid from the bacteria demineralizes the hydroxyapatite crystals, calcium and phosphorus are released, allowing for the precipitation of more crystals which fall deeper into the dentinal tubule. These crystals form a barrier and slow the advancement of caries. After these protective responses, the dentin is considered sclerotic.
Fluids within dentinal tubules are believed to be the mechanism by which pain receptors are triggered within the pulp of the tooth. Since sclerotic dentin prevents the passage of such fluids, pain that would otherwise serve as a warning of the invading bacteria may not develop at first. Consequently, dental caries may progress for a long period of time without any sensitivity of the tooth, allowing for greater loss of tooth structure.
Tertiary dentin
In response to dental caries, there may the production of more dentin toward the direction of the pulp. This new dentin is referred to as tertiary dentin. Tertiary dentin is produced to protect the pulp for as long as possible from the advancing bacteria. As more tertiary dentin is produced, the size of the pulp decreases. This type of dentin has been subdivided according to the presence or absence of the original odontoblasts. If the odontoblasts survive long enough to react to the dental caries, then the dentin produced is called "reactionary" dentin. If the odontoblasts are killed, the dentin produced is called "reparative" dentin.
In the case of reparative dentin, other cells are needed to assume the role of the destroyed odontoblasts. Growth factors, especially TGF-β, are thought to initiate the production of reparative dentin by fibroblasts and mesenchymal cells of the pulp. Reparative dentin is produced at an average of 1.5 μm/day, but can be increased to 3.5 μm/day. The resulting dentin contains irregularly-shaped dentinal tubules which may not line up with existing dentinal tubules. This diminishes the ability for dental caries to progress within the dentinal tubules.
Treatment

An amalgam used as a restorative material in a tooth.
Destroyed tooth structure does not fully regenerate, although remineralization of very small carious lesions may occur if dental hygiene is kept at optimal level. For the small lesions, topical fluoride is sometimes used to encourage remineralization. For larger lesions, the progression of dental caries can be stopped by treatment. The goal of treatment is to preserve tooth structures and prevent further destruction of the tooth.
Generally, early treatment is less painful and less expensive than treatment of extensive decay. Anesthetics — local, nitrous oxide ("laughing gas"), or other prescription medications — may be required in some cases to relieve pain during or following treatment or to relieve anxiety during treatment. A dental handpiece ("drill") is used to remove large portions of decayed material from a tooth. A spoon is a dental instrument used to remove decay carefully and is sometimes employed when the decay in dentin reaches near the pulp. Once the decay is removed, the missing tooth structure requires a dental restoration of some sort to return the tooth to functionality and aesthetic condition.
Restorative materials include dental amalgam, composite resin, porcelain, and gold. Composite resin and porcelain can be made to match the color of a patient's natural teeth and are thus used more frequently when aesthetics are a concern. Composite restorations are not as strong as dental amalgam and gold; some dentists consider the latter as the only advisable restoration for posterior areas where chewing forces are great. When the decay is too extensive, there may not be enough tooth structure remaining to allow a restorative material to be placed within the tooth. Thus, a crown may be needed. This restoration appears similar to a cap and is fitted over the remainder of the natural crown of the tooth. Crowns are often made of gold, porcelain, or porcelain fused to metal.

A tooth with extensive caries eventually requiring extraction.
In certain cases, root canal therapy may be necessary for the restoration of a tooth. Root canal therapy, also called "endodontic therapy", is recommended if the pulp in a tooth dies from infection by decay-causing bacteria or from trauma. During a root canal, the pulp of the tooth, including the nerve and vascular tissues, is removed along with decayed portions of the tooth. The canals are instrumented with endodontic files to clean and shape them, and they are then usually filled with a rubber-like material called gutta percha. The tooth is filled and a crown can be placed. Upon completion of a root canal, the tooth is now non-vital, as it is devoid of any living tissue.
An extraction can also serve as treatment for dental caries. The removal of the decayed tooth is performed if the tooth is too far destroyed from the decay process to effectively restore the tooth. Extractions are sometimes considered if the tooth lacks an opposing tooth or will probably cause further problems in the future, as may be the case for wisdom teeth. Extractions may also be preferred by patients unable or unwilling to undergo the expense or difficulties in restoring the tooth.
Prevention

Toothbrushes are commonly used to clean teeth.
Oral hygiene
Personal hygiene care consists of proper brushing and flossing daily. The purpose of oral hygiene is to minimize any etiologic agents of disease in the mouth. The primary focus of brushing and flossing is to remove and prevent the formation of plaque. Plaque consists mostly of bacteria. As the amount of bacterial plaque increases, the tooth is more vulnerable to dental caries. A toothbrush can be used to remove plaque on most surfaces of the teeth except for areas between teeth. When used correctly, dental floss removes plaque from areas which could otherwise develop proximal caries. Other adjunct hygiene aids include interdental brushes, water picks, and mouthwashes.
Professional hygiene care consists of regular dental examinations and cleanings. Sometimes, complete plaque removal is difficult, and a dentist or dental hygienist may be needed. Along with oral hygiene, radiographs may be taken at dental visits to detect possible dental caries development in high risk areas of the mouth.
Dietary modification
For dental health, afrequency of sugar intake is more important than the amount of sugar consumed. In the presence of sugar and other carbohydrates, bacteria in the mouth produce acids which can demineralize enamel, dentin, and cementum. The more frequently teeth are exposed to this environment, the more likely dental caries are to occur. Therefore, minimizing snacking is recommended, since snacking creates a continual supply of nutrition for acid-creating bacteria in the mouth. Also, chewy and sticky foods (such as dried fruit or candy) tend to adhere to teeth longer, and consequently are best eaten as part of a meal. Brushing the teeth after meals is recommended. For children, the American Dental Association and the European Academy of Paediatric Dentistry recommend limiting the frequency of consumption of drinks with sugar, and not giving baby bottles to infants during sleep. Mothers are also recommended to avoid sharing utensils and cups with their infants to prevent transferring bacteria from the mother's mouth.
It has been found that milk and certain kinds of cheese like cheddar can help counter tooth decay if eaten soon after the consumption of foods potentially harmful to teeth. Also, chewing gum containing xylitol (wood sugar) is widely used to protect teeth in some countries, being especially popular in the Finnish candy industry. Xylitol's effect on reducing plaque is probably due to bacteria's inability to utilize it like other sugars. Chewing and stimulation of flavour receptors on the tongue are also known to increase the production and release of saliva, which contains natural buffers to prevent the lowering of pH in the mouth to the point where enamel may become demineralised.

Common dentistry trays used to deliver fluoride.
Other preventive measures
The use of dental sealants is a means of prevention. A sealant is a thin plastic-like coating applied to the chewing surfaces of the molars. This coating prevents the accumulation of plaque in the deep grooves and thus prevents the formation of pit and fissure caries, the most common form of dental caries. Sealants are usually applied on the teeth of children, shortly after the molars erupt. Older people may also benefit from the use of tooth sealants, but their dental history and likelihood of caries formation are usually taken into consideration.
Fluoride therapy is often recommended to protect against dental caries. It has been demonstrated that water fluoridation and fluoride supplements decrease the incidence of dental caries. Fluoride helps prevent decay of a tooth by binding to the hydroxyapatite crystals in enamel. The incorporated fluoride makes enamel more resistant to demineralization and, thus, resistant to decay. Topical fluoride is also recommended to protect the surface of the teeth. This may include a fluoride toothpaste or mouthwash. Many dentists include application of topical fluoride solutions as part of routine visits.
Furthermore, recent research shows that low intensity laser radiation of argon ion lasers may prevent the susceptibility for enamel caries and white spot lesions. Also, as bacteria are a major factor contributing to poor oral health, there is currently research to find a vaccine for dental caries. As of 2004, such a vaccine has been successfully tested on animals, and is in clinical trials for humans as of May 2006.